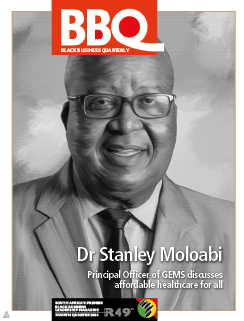
Unlocking the benefits of a high-performing Government Employees Medical Scheme (GEMS): Ensuring quality care for all
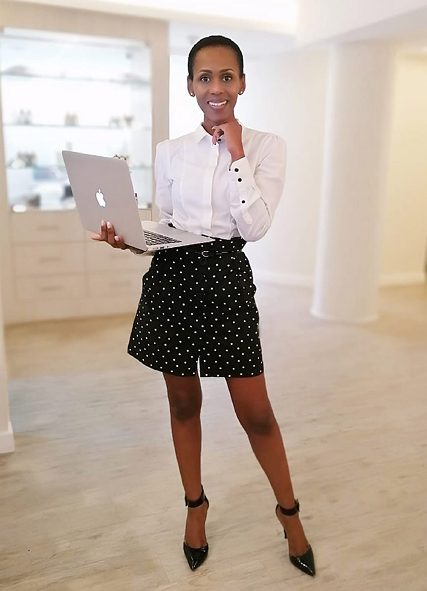
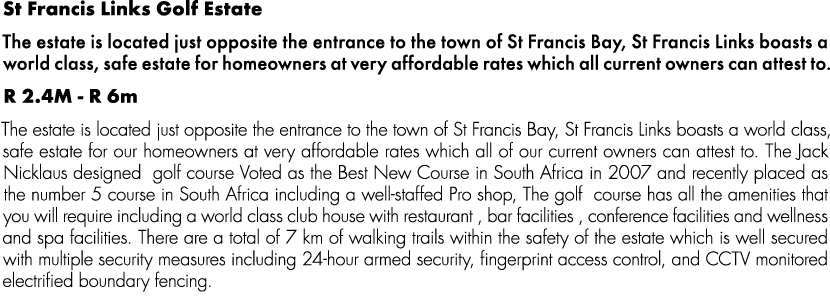
Principal Officer
Dr Stanley Moloabi takes us behind the scenes of the Government Employees Medical Scheme (GEMS) and gives us some important insight into how it manages to function so well.
In an era where healthcare is becoming increasingly complex and costly, having access to quality, affordable medical cover is more important than ever. While many medical schemes face challenges in balancing comprehensive care with rising costs, some stand out for their exceptional performance, proving that it is possible to offer both value and high-quality service.
The Government Employees Medical Scheme (GEMS) is one such medical scheme that has not only met but exceeded the expectations of its members. Focusing on innovation, member satisfaction, and financial sustainability, GEMS has set a new benchmark for what can be achieved in the healthcare sector.
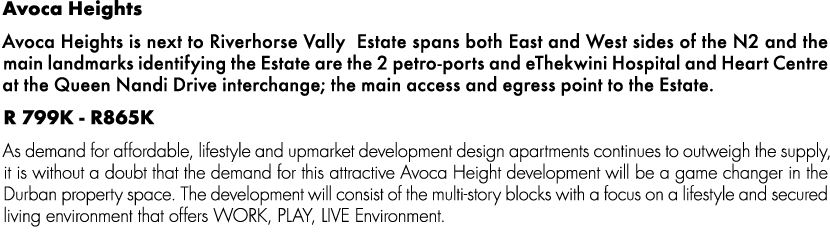
Since its registration on 1 January 2005, specifically to meet the healthcare needs of government employees, GEMS has grown to greater heights, living up to its mission of providing all members with equitable access to affordable and comprehensive healthcare and promoting member well-being. With just two years away from two decades in existence, the scheme is South Africa’s largest restricted medical scheme, with over 800 000 principal members and two million beneficiaries.
GEMS is an excellent, sustainable, and effective medical scheme that drives transformation in the healthcare industry, aligned with the principles of universal healthcare coverage. The benefit option design process is part of the business activities and is a value driver aligned with the strategy. The benefit options were designed using a rigorous analytical approach considering the Council for Medical Scheme requirements, member affordability, the scheme's strategic direction, stakeholder engagement inputs, and results, as well as benefit design assessment.
GEMS Principal Officer, Dr Stanley Moloabi, revealed the key factors behind its success and how it continues to shape the future of medical coverage for its growing members. GEMS as an organisation subscribes to corporate governance to ensure accountability, transparency, and ethical behaviour. Strong corporate governance has seen GEMS improve stakeholder confidence, fostering better decision-making, mitigating risks, and enhancing its overall performance and sustainability. The Board meets regularly and monitors the performance of the Scheme’s employees, administrators, and other contracted service providers. The Board addresses various issues and ensures that discussions on strategy, policy, risk management, fraud management, and operational performance are critical, informed, and constructive.
Maintaining financial sustainability in a tough economy
Acknowledging that the medical Scheme has experienced both challenges and achievements, Dr Moloabi explained that the scheme was able to “maintain sufficient funding to cover its obligations without needing excessive financial intervention or threatening the affordability of its services to members”. This long-standing achievement by the scheme is owed to the prudent financial management managing the Scheme’s finances with caution, foresight, and integrity. This included ensuring that the non-healthcare costs are kept low at 5% and below compared to the industry which spends in the region of 8-9%. Healthcare costs, however, do come with their challenges and often are above what has been budgeted for.“To address this,” Dr Moloabi says, “the Scheme had to come up with a multifaceted approach to ensure that we try and lessen the increasing costs. The interventions put in place to lessen the costs, among others, include a managed care intervention which happens at a level of authorisation, as well as educating members that when they access healthcare benefits, it must be for clinically appropriate and necessary healthcare.” Another intervention used to manage healthcare costs which was a huge success is the introduction of care coordination.
This was done through the introduction of an Efficiency Discount Option (EDO), Emerald Value Option (EVO) which is a sub-option of the Emerald Option (Benefit Plan). The two options have the same benefits, and the difference is that EVO is cost-effective, but through care coordination which results in downstream costs being managed more closely. The care coordination approach allows each family to nominate a family doctor within the doctor's network, which ultimately minimises doctor-hopping and self-referral to secondary health care.
Dr Moloabi shared how the members utterly rejected the introduction of these cost-cutting measures at the first attempt to introduce it in 2015, but through corrective steps of wide consultation in 2017, the care coordination was welcomed by the members. As the saying goes, ‘the best view comes after the hardest climb’. To date, this is a proven contributor to the Scheme's financial sustainability. This is proven by the rate at which EVO and Tanzanite options are growing.
“Using the size and reach to negotiate competitive rates with service providers and healthcare providers, we perform a comprehensive analysis annually to assess benefit options, focusing on those like the GEMS options. The analysis also shows how GEMS compares to similar medical Scheme options from the five largest open and restricted medical Schemes. For example, GEMS Tanzanite One members, on average enjoy a 97% discount for each Rand spent on contributions (after allowing for the public service subsidy) than they would have experienced on these competing options. Each of the GEMS options was found to be more cost-effective than its competitors. On average we calculate the relative value for money on GEMS options to be 66% higher than the competing options.”
Financial management and operations
Undeniably, the cost of healthcare has gone up. To keep up with evolving economic changes, and rising costs, GEMS strategic framework aligns functional strategies and strategic projects and programmes to support the overarching Scheme’s strategic intent to pursue achieving UHC through strategic partnerships.
“This ensures clarity on the prioritisation of initiatives for successful execution. These strategies and programmes leverage our competitive advantages—our market-leading Tanzanite One basic benefit option and affordable access to high-quality healthcare for all our members—and build competitive advantage across governance, financial, and healthcare objectives,” Dr Moloabi says.
“The rise of non-communicable diseases (NCDs), such as hypertension, diabetes, and trauma, underscores the importance of health risk management programs. These programs are designed to assist our members in preventing the escalation of these conditions. By effectively managing these diseases, we aim to ensure better control, which reduces the need for health services and, ultimately, health-related costs.
Before the 2020 pandemic, our management programs yielded remarkable results. However, during the pandemic, reduced human movement led to fewer consultations, except for a few cases requiring hospitalisation. Unfortunately, we faced significant challenges post-pandemic as health costs began to rise again.”
Following a remarkably close to no increase in members' contribution over the past two to three years, the Scheme was using reserves to cover health costs of over R10 billion. To remain financially viable and to manage the risk of depleting the reserves, this has resulted in the need to adjust member contributions with a much higher increase percentage of 9.5% in 2024 to ensure that GEMS stays financially viable. Due to an uptick in health costs and the need to manage financial decline risks, with the next financial year increase, members can expect to pay a higher percentage than the current one.
“When we communicate the increase, what is at the centre of our messages is to ensure that our members understand that this is done for good reason and to sustain the financial viability of the Scheme. The health costs forecast is clear and for the Scheme to meet the members' healthcare needs for 2025 the contribution increase must be affected,” Dr Moloabi emphasises.
Over and above the rising health costs, which are exacerbated by increased utilisation and slow-paced economic growth, fewer younger generations are entering the job market. The high number of increased age members is a contributor to the high health cost. In a good economic environment, the younger members subsidise the health costs of older members, as inevitably the older one gets, the higher the health cost. Another contributing factor to a higher health cost is supplier-induced demand (SID), where health providers are charging more than what is deemed standard practice. However, GEMS has to a certain degree managed this through the doctor's network, but there are those in the industry who still charge more compared to the agreed rate in the network.
Risk management to remain financially viable
At a governance level, the Board annually performs a strategic risk assessment to coincide with the review of strategic plan objectives and targets. A standing committee is mandated to monitor strategic risks that exceed risk tolerance and risk-bearing capacity and are within risk appetite. Over and above risk management in the context of operations, health risk management is important and employed to identify, assess, and manage the risks that affect the health and financial sustainability of GEMS. To ensure that the healthcare that members are getting is appropriate, being strict in protocols, evidence-based protocols used to treat patients, is vital.
“The Scheme experienced an increase in claims costs in the aftermath of COVID-19. The claims loss ratio increased from 89% in 2019 to 96% in 2022 and 102% in 2023. Hospital admission rates across most options have also increased and are more closely in line with the pre-COVID-19 experience. These trends are expected to continue in the medium term given the scheme’s burden of disease. More than 43% of the Scheme’s principal members are living with one or more chronic conditions. The claims costs incurred by members living with three chronic conditions are generally more than double the costs incurred by members with just one such condition. Also notable is the continuous increase in mental health claims costs for more members than was the case pre-COVID-19. The Scheme will continue to enhance and advance preventive and primary healthcare benefits for its members to mitigate the impact of the disease burden in the medium- to long-term. Mental health benefits and programmes will endure to support members’ well-being outcomes. These are being addressed using the GEMS product development and benefit design processes,” Dr Moloabi explains.
“What has and continues to help us manage health risks is having health risk management programmes. Namely, a high-risk member management programme within which patients are identified as high-risk and are monitored. Monitoring and managing claims ensures they are legitimate and within expected norms. This involves regular audits, medical reviews, and monitoring for fraud or over-utilisation of healthcare services. Secondly, engaging with members to make them aware of their health risks and encouraging behaviour changes that can improve health outcomes. This includes educating on managing chronic conditions and offering personalised healthcare support.”
Responding to the possibility of a risk where members may not take kindly to the planned contribution increases, Dr Moloabi says he is confident that the strategic stakeholder relationship and engagement strategy that is in place, aimed at ensuring meaningful feedback for stakeholders, will suffice.
GEMS and the South African National Health Insurance
“GEMS supports the implementation of the National Health Insurance (NHI) to the extent that even the corporate strategy review always makes provision and assesses their state of readiness should the NHI be implemented. At the centre of our support is ensuring that the NHI is implemented in a responsible manner that will make it reach its goals. In our plan to support this we will participate throughout the process and not play a spectator role, we plan to collaborate and partner with the NHI to reach its intended goals,” says Dr Moloabi.
“The evolving National Health Insurance policy environment necessitated the development of scenarios, identifying the Scheme’s competitive positioning and advantage to drive its strategic direction. An analysis of the current Universal Health Coverage (UHC) which is global and the NHI (local) landscape was conducted to identify implications for GEMS. Views on the impact of the NHI Act on GEMS were solicited from internal and external stakeholders. Detailed analyses were conducted on the Scheme’s competitive environment and GEMS' performance against peers.
“This highlighted strengths for the Scheme to leverage opportunities and weaknesses needing improvement. Additionally, a gap analysis conducted in 2022 highlighted the need to strengthen innovation capability and adopt sustainability best practices to further improve the Scheme’s reputation as a responsible corporate citizen. In anticipation of further NHI developments, the Scheme has enhanced its strategic thrust: To be a strategic partner in pursuit of UHC. Three scenarios were crafted showing outer extremes and a middle road possible in NHI implementation: Initial implementation, partial implementation, and full implementation. These scenarios informed the development of three strategic approaches for the Scheme, namely growth, diversification, and partnerships, which present opportunities to remain relevant, competitive, and sustainable in the short-, medium- and long term.”
Looking ahead five years from now
“Our key focus for 2025 and beyond is a response to stakeholder concerns on the quality of engagements and perceived low transparency. A new key performance indicator will seek to increase stakeholder trust through outcomes-based engagements and demonstrate how stakeholder inputs shape our decision-making,” he admits.
Increased and inclusive stakeholder engagement
“Our annual stakeholder engagement plan will become risk-led, which requires us to identify risks and opportunities for each stakeholder. The focus area requirements will be met in a revised inclusive and holistic stakeholder strategy and engagement plan aligned to each NHI implementation scenario. Engagement topics for 2025 will remain NHI, the insourcing programme, Board composition, factors influencing contribution increases and benefit enhancements, implementing the findings and recommendations of the Section 59 Investigation, and results achieved in our quest to be affordable, such as co-payments,” he emphasises. For members, Dr Moloabi says the focus will be on improving digital platforms to drive increased usage. Engagement topics for members will remain benefit options and encourage optimal access to and usage of benefits. Ongoing improvement in claims administration and improving satisfaction levels will drive engagement with healthcare providers. On-site training for provincial health departments will be extended to improve public sector revenue. The rapid move towards sustainability mainstreaming and ESG post-pandemic era holds significant implications for the Scheme’s performance and disclosures. An end-to-end ESG framework is essential to demonstrate commitment to responsible and sustainable business practices and responsiveness to stakeholder expectations.
Risk universe
GEMS strategy is to manage risks that may affect business sustainability in internal and external environments. “Our risk management process, also covering our outsourced service providers, enables us to work towards managing our risk profile within our risk appetite. Through combined assurance, our management and Board of Trustees transparently report on our performance to stakeholders. Our risk universe illustrates the risk environment in which we operate that constitutes the sources of risks to which we may be exposed,” he states. “This represents the minimum scope of application of our risk management processes and is segmented into three levels, namely purpose, strategy, and operational realities. We continuously review and update the risk universe as an accurate representation of our strategic and operating environments. We anchor each identified risk in the relevant operational, strategic, and purpose activity to enable decision-makers to contextualise and understand the interrelationships between our activities and the risks we face.”
Growing the Scheme's membership
“Growing and expanding GEMS is of great importance, not just for the employees themselves, but for the broader healthcare system and the nation. We believe that growing the Scheme can create economies of scale, where the increasing number of members reduces the average cost per member, making the Scheme even more affordable in the long term. While understanding the economic factors of the country such as the slow growth resulting in fewer and fewer people joining government employees, we had to come up with approaches to continue to see membership growth,” he continues.“To date, the Scheme records new membership of between 1 200 to 2 000 members joining monthly, and these numbers are owed to the Scheme's decision to open the membership to other institutions that are organs of the state, such as the Chapter 9 institutions and Public Entities. This goes to show how much GEMS will remain a medical scheme of choice. Even in a situation where these institutions do not necessarily qualify for the government subsidy, they still choose GEMS. These are not just numbers; they are contributors to the financial viability of the Scheme and its future growth which will address the claims pressure which remains a concern.”
Emerging healthcare trends, digital healthcare innovations
“In advancing our position in an evolving and dynamic healthcare ecosystem, GEMS innovation value is central to remaining relevant and sustainable. This includes new thinking and ideas to deliver superior and meaningful value for members and stakeholders,” Dr Moloabi says. “The Scheme’s digital transformation strategy includes strategic priorities such as the development of best of breed digital platforms capability among others. These digital systems will handle the data used to enhance decision-making and ultimately improve service and benefits to members.
These advancements can enhance the Scheme's effectiveness, improve patient outcomes, reduce costs, and streamline administrative processes. We believe that incorporating emerging healthcare trends and digital innovations can significantly enhance the value of GEMS for its members. By leveraging technologies like AI, wearables, and blockchain, GEMS can provide more efficient, personalised, and accessible healthcare. These innovations will not only benefit individual health outcomes but also contribute to the broader goal of reducing healthcare costs and improving the sustainability and scalability of healthcare services for the members.”
GEMS and responsible citizenship
GEMS priorities do not lie only in increasing numbers and being a leading medical aid scheme, but also take matters of responsible citizenship as fundamental for the well-being of society. By championing this commitment, GEMS encourages individuals to actively contribute to social, economic, and environmental sustainability.
Dr Moloabi concludes: “We believe that, through active participation, ethical behaviour, and a commitment to justice, responsible citizens help strengthen democratic systems, promote unity, and ensure a stable and prosperous future. As the country continues to face complex challenges, such as poverty, climate change, and inequality, the importance of responsible citizenship has never been more critical. GEMS is proud that for many years we have been able to support communities and the health space with items such as donating medical equipment for clinics in need and school shoes for schools, renovation of clinics and medical and school facilities, and touching lives in collaboration with the employer.” 
Lavhelesani Mainganye is a PRISA accredited communication practitioner with considerable experience in the field.

















































































-flags.gif)























































































-law-video.gif)